Uterine Fibroids
What are uterine fibroids?
Uterine fibroids are non-cancerous tumors that grow on or within the muscle tissue of the uterus.
Up to 80% of women develop fibroids at some point in their lives.
You are at a higher risk of developing them if you are Black and have fibroids run in your family.
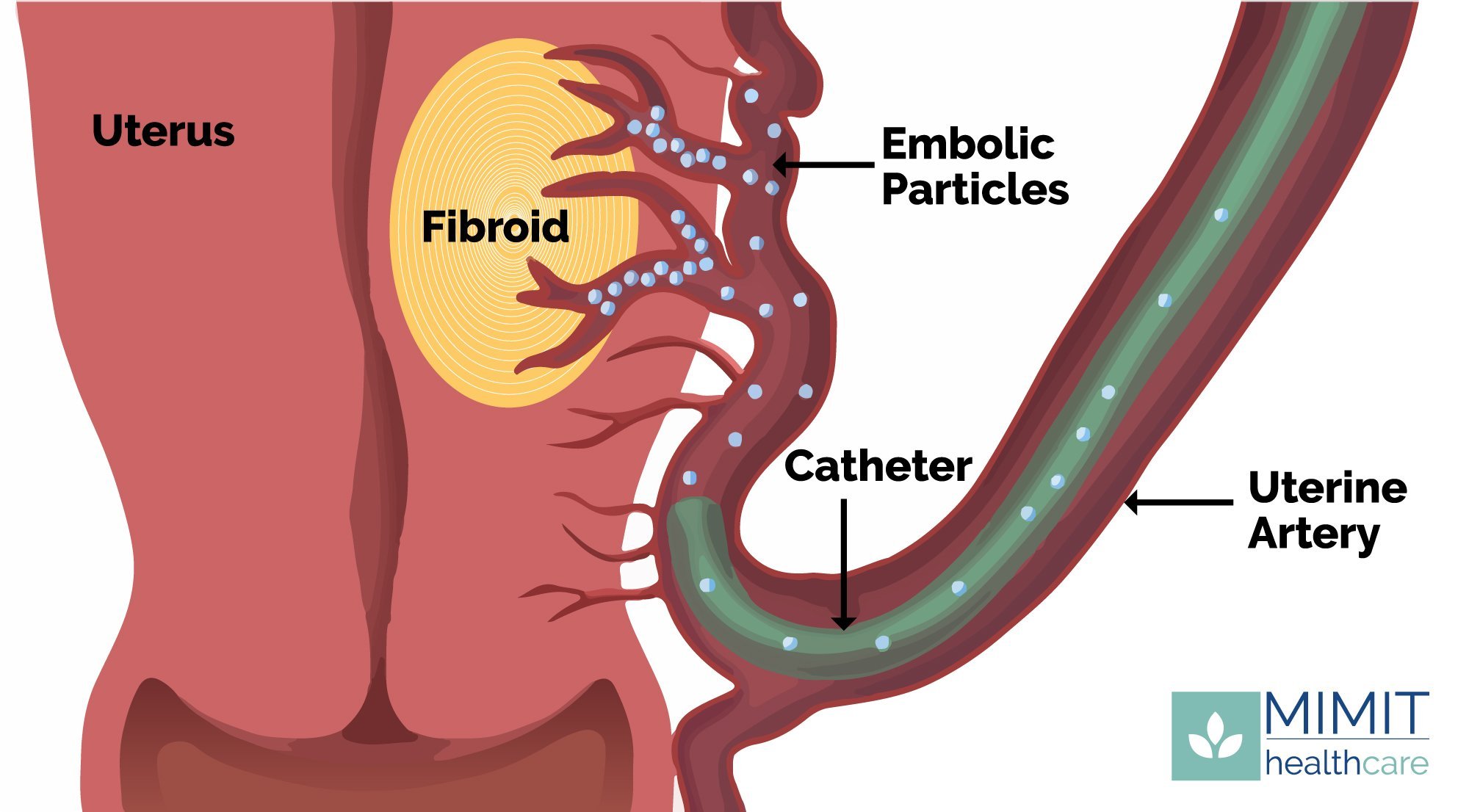
Uterine fibroid embolization is a common treatment option, which cuts off the blood supply to the tumor, leading it to shrink over time.
Uterine fibroid symptoms
Uterine fibroids can cause a variety of symptoms, but the most common symptom is heavy menstrual bleeding and pelvic pain. Other symptoms include:
Pain during intercourse
Anemia due to heavy bleeding
Lower abdominal pain/swelling, which can be mistaken as weight gain or pregnancy
Frequent urination
Difficulty emptying the bladder
Constipation
Backache or leg pains
Sometimes there aren't any symptoms at all!
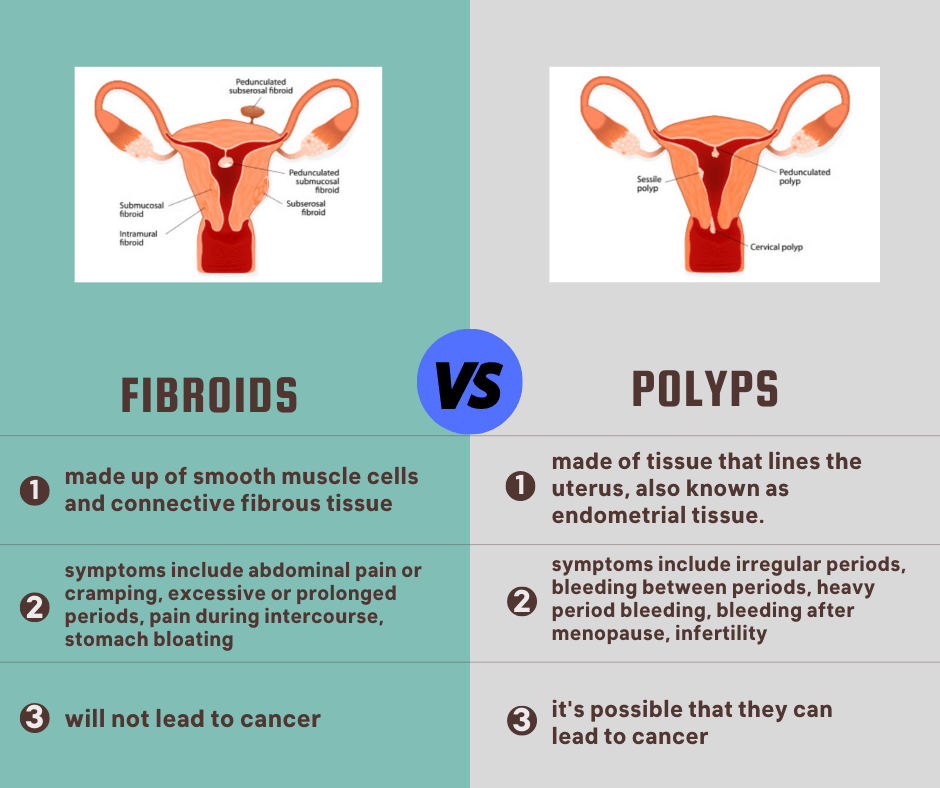
What are the different types of fibroids?
-
Subserosal
Subserosal fibroids grow on the outer wall of the uterus and can grow quite large.
-
Submucosal
Submucosal fibroids form under the lining of uterine cavity.
-
Pedunculated
Pedunculated fibroids actually appear as a peduncle, which is an attaching stalk of sorts.
-
Intramural
Intramural fibroids which grow within the wall of the uterus.
-
Exophytic
Exophytic fibroids, which jut outwards from the uterus into the cavity, are often referred to as ‘proud’ fibroids.
Causes of uterine fibroids
Doctors don’t yet know the cause of fibroids. However, the following could increase your risk of developing fibroids:
Genetics
If fibroids runs in your family, you’re more likely to develop them, too.
Hormones, specifically estrogen
Estrogen is the chemical that makes your uterine lining thicken at each period. Therefore, prolonged use could increase your likelihood of developing fibroids.
Risk factors for developing fibroids
Women 35-years-old and older have the highest risk, but remember that fibroids can develop before then.
Fibroids can and do occur in women under the age of 35, even as young as the early 20s.
Women who are Black are also at-risk.
Some statistics indicate that up to 80% of African-American women will develop uterine fibroids.
Those who have fibroids run in their family are at an increased risk, too.
Uterine fibroid diagnosis
Ultrasound
Fibroids develop in the uterus, so ultrasound imaging is a reliable way to visualize any potential members growing inside a woman’s body.
This type of ultrasound is also useful for determining and understanding the size, shape, and location of the fibroid so that treatment options can be more fully explored.
Ultrasound has become a go-to option for initial diagnosis of fibroids because it is painless and cost effective, making it accessible for anyone who might have concerns about any possible abnormalities in the uterus.
MRI
While ultrasound imaging can diagnose fibroids, it does not offer the 3-D resolution of an MRI. The higher-resolution MRI, can not only offer a clearer image of the fibroids, but can show their size, number, and location. An MRI will often see things that were not seen on the ultrasound exam, too.
Minimally invasive treatment for fibroids
Uterine fibroid embolization is a minimally invasive procedure that treats fibroids. You get to keep your uterus and avoid the risks of a hysterectomy. By using just a catheter, an interventional radiologist cuts off the blood supplying the fibroids, causing them to shrink and disappear over time.
Dr. Chopra answers frequently asked questions about fibroids
Still want to learn more? Dr. Chopra answers the most asked questions about fibroids.